I often find myself writing an article when I’m repeating a similar conversation to patients. This current idea has been a harder sell I feel. I don’t think it’s the only player by a long stretch but I do feel it’s way more common than we realise and rarely considered. It may also be just a partial player. I’ve said in many articles before that back pain and arthritis are multi factorial issues with rarely one cause. I’m going to make a strong case for one cause rarely considered (including evidence and studies) and you can draw your own conclusions. Or at least just be introduced to a new idea. As a caveat, this is more for those with arthritis being the primary problem and/or those with persistent back pain that never resolves fully. If you go long stretches without back pain and have a sudden new episode following movement this explanation is unlikely in that scenario. If you have chronic back stiffness and pain, or arthritis, that responds well to movement, manipulation (hint your back isn’t poorly aligned) and anti inflammatory medications, this could be worth considering. This was certainly my own story for many years.
Bacteria and the great human ecosystem
Most people don’t think of ourselves as having bacteria within our bodies unless we are sick. We think of bacteria as something we must avoid so we wash our hands and try not to touch surfaces on indoor public spaces. What people often don’t realise is that we are an ecosystem. We actually have more bacterial cells within us than our human cells. This is normal. Unfortunately, as we age the ecosystem within us can start to take over more and more. A healthy immune system can handle a certain amount of this, but it has limits. If our immune system is continually acting on bacteria throughout the body, the result is inflammation. That’s inflammation wherever the immune system has responded. For some it’s hands and feet. For others the little joints throughout the spine. These areas have a high number of capillaries and as the cell wall is smaller the blood vessels are designed to leak more. More leakage = more bacteria escaping from the blood.
Inflammation recap
We’ve talked inflammation many times before but the gist of it is an inflamed body has problems. It’s actively more painful to move. It’s also stiffer due to a process called fibrosis. Fibrosis and inflammation are very tightly linked. Inflammation precedes fibrosis. If fibrosis persists, the body lays down calcium as a protective response. The combination of fibrosis and calcification is in effect osteoarthritis. When we look at X-rays of someone with arthritis we see lots of whitening which is calcium being laid down. What would happen when we add mechanical forces to this changed tissue? Nothing good. These joints accumulate wear and tear much faster and more severely. Repetitive forces on fibrotic, calcifying cells will not end well.
But doesn't bad biomechanics cause back pain?
Biomechanics do feature, they just shouldn’t be considered the primary driver. Have you ever wondered why some people can run marathon after marathon but others walk to the shops and have sore knees? Does the marathon runner have honed to perfection knee hinge biomechanics or is there something more at play? I lean strongly towards the latter.
The biomechanics absolutists could argue that the marathon runner is lighter and has less weight and force through the knee joint, they are stronger and more conditioned for running. They are but is this really the whole story? I had a similar conversation with my own Dad a GP in the UK. He lost 5Kg from changing his diet from suggestions I made and was able to run for the first time again in 10 years. He concluded (imo wrongly) that the extra 5Kg he was carrying compressed his knees too much and caused his arthritic pains. I had to disagree and suggested the weight loss was more a red herring and he had more s no o changed his physiology into being less inflamed ie less immune active and less bacterial burden. He also had a healthier metabolism so this was repairing better. I proposed that if he stayed eating the way he was and continued taking the turmeric he was taking, he could wear a 5Kg weight-vest all week and his pain wouldn’t come back. He never did the experiment sadly.
The research
To make my case stronger I looked into the research. The first article reviews the literature of the relationship of the gut microbiome and osteoarthritis. They conclude an association between diet, gut dysbiosis and osteoarthritis severity. https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC8675674/ This one looks at the data re the contribution of bacterial infection to chronic low back pain and its treatment with antibiotics. Two randomized, controlled clinical trials evaluating oral antibiotics in patients with CLBP indicate that for certain subsets of patients, the reduction in pain and disability achieved with antibiotic therapy may be significant. They also discuss the idea that structures such as disc have a microbiome.This was touched upon in this podcast. The future of spinal injury treatment and the surprising connection between bacteria, your microbiome and spinal disc degeneration; https://youtu.
be/eGuwoeGVFNA?si= .X50eT5Z2nIRqH6qR The next article is https://pubmed.ncbi.nlm.nih.
gov/33610802/ , another review of the data with proposed mechanisms. It suggests gut microbiota modulation can also be proposed as a new therapy for OA.https://www.frontiersin.org/
articles/10.3389/fcimb.2022. This paper also leads us into mechanisms and ways to improve this pathology. It also also touches upon another important area of metabolic health and energy metabolism. I would say in simple terms this relates to how well the inflammation from the immune response is repaired and resolved. Someone with good metabolic health may still have the immune response as discussed but their ability to clear the inflammation and fibrosis that results is superior to someone with poor metabolic health.812596/full The following podcast goes into more detail about the connection between metabolic health and having healthy structures in your body; https://youtu.be/
N4ZlZBbu6tY?si= 1XFIhGVE1EGuLwtG
Does a healthy metabolism help?
I would say from a personal experience, when I had my pattern of back pain over 8 years ago I would actually recover pretty well. I had a pretty healthly metabolic system but just a chronically active personal immune response. It just became too repetitive over time. I would have an immune response and subsequent inflammation, my biology would clear and repair the area and wait for the next response. Rinse and repeat. My lower back and mid back would be persistently stiff and ache but if I exercised and moved consistently it would resolve. Every few weeks I would have my colleague Scott manipulate the stiff part of my back. Once I figured out how to avoid the immune and inflammation response I no longer had the need to stretch, move or have manipulation to feel better. I could also stop taking anti inflammatory medications when I was having a bad day with it. It’s this pattern I see so frequently with patients. We do however have evidence that within a metabolically unhealthy patient with high BMI we are more likely to have a less favourable microbiome. Obese individuals show to possess a lower proportion of Bacteroidetes and higher levels of Firmicutes than their lean counterparts. It appears hard to have a healthy microbiome if you have metabolic issues as seen in this article: https://www.ncbi.nlm.nih.gov/
pmc/articles/PMC3427212/#:~: .text=It%20was%20revealed% 20that%20the,established%20in% 20previous%20murine%20studies
Practical tips
Now moving more into practical tips and ideas around treatment. The paper earlier on mechanisms at play suggests a few ideas; probiotics and prebiotics, diet and nutraceuticals, exercise, and the last I am not so keen on, fecal microbiota transplantation. I believe diet is probably the best to start with. Let’s introduce a new idea here. The migration of bacteria and their metabolites from our digestive tract into our bloodstream. As odd as it sounds, the approach I take with my own diet is to minimise this migration. There are certain foods that are harder to digest and thus cause a stronger interaction with our microbiome ie. We require our bacteria to break it down for us. This can result in more problematic metabolites produced from bacterial action. There are also certain foods that appear to increase intestinal permeability in some individuals. Thus, this combination can increase the migration of gut bacteria and metabolites into our blood stream. I feel the article below covers this pretty well. My previous blog article on a simple gut protocol could also help. The article is mostly suggesting a way of eating that reduces the metabolites of bacteria crossing into the bloodstream and circulating through the body. I also see no major risk in trying a good probiotic and increasing time spent outdoors which has been shown to have a positive modulation effect on the microbiome. Lots of sunlight due to the benefits of UV and red light. Exercise certainly helps modulate inflammation too.
https://drruscio.com/leaky-
gut-food-list/
Are Antibiotics the obvious solution?
The next question to be considered is if bacteria are the issue why not just use an antibiotic? Well this can get tricky. Some antibiotics kill off bacteria in the body that may not be involved in arthritic changes in our bodies and may be helping balance out the ones that are. Certain bacteria produce metabolites that are anti-inflammatory or have positive effects on an individuals biology. It’s hard to target exactly the ones we think are causing issues. This is why when I looked into the studies on this it’s fairly inconclusive. I think a low dose of some of the older schools tetracyclic antibiotics such as minocyclin look promising but I just think this approach will be far too unpredictable and individual. It may work for some. It may not work for others. I strongly lean towards diet and lifestyle changes as a much safer overall approach.
Testing?
Our technology has yet to really get up to speed with whole body bacterial analysis. Even when we do microbiome testing we really are in the infancy of what to do about it. We can definitely consider clinical symptoms as discussed earlier - chronic stiffness, easy to injure, responds well to anti-inflammatory meds, improves with periods of diet medications. For doctors reading, I’d also consider some basic patterns within blood markers. None of these are definitive but could indicate chronic immune activation; lower white blood cells - particularly neutrophils, excessively high HDL ie above 2.0, CRP above 1.0, low Vit D despite adequate sun exposure, low thyroid function, low albumin, poor metabolic blood markers. I think patterns are more likely be more useful than individual markers.
Summary
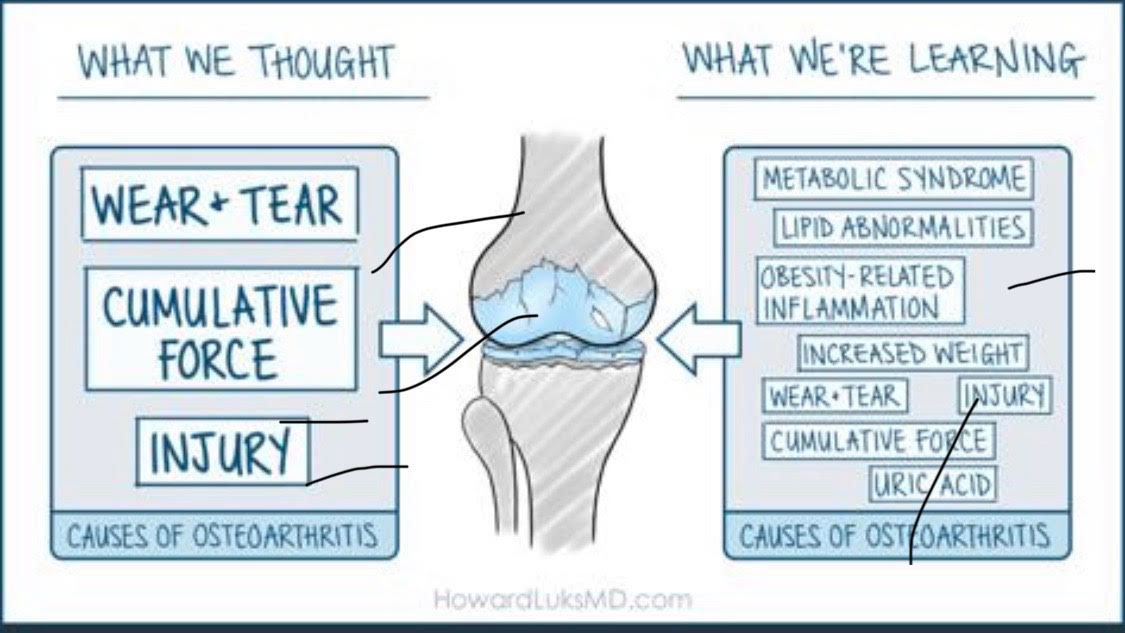
We are still learning more each day with how different systems in our biology may be interacting with each other. Images like this are popping up in conventional physio circles but we may still have a wait to get the research to match what we are starting to suspect. As a patient you just need to be curious to try a different approach. Maybe it’s not just genetics and faulty biomechanics? If I didn’t have this same curiosity I’d still be stretching obsessively, taking pills and begging my colleagues to crack my back.
Making the case for bacteria - a misunderstood, unexpected player in osteoarthritis and chronic back pain.
Posted By Jamie Page
06/08/2024
